What causes Postpartum Urinary Retention?
Sometimes, women experience something called postpartum urinary retention, or voiding dysfunction. This can happen during the first couple of days after delivery, whether it was a vaginal or cesarean birth. It can happen after childbirth, foley catheter removal, anesthesia, or perineal trauma. Postpartum urinary retention can occur two ways: when the bladder is unable to release any urine, or when there is more than 200mL (a little less than 1 cup) left in the bladder after urinating. The average bladder holds around 400-600mL of urine. This is a little over 2 cups, or a half of a liter. At around 500mL, you may feel some hardness above the pubic bone. If the bladder fills to around 1000mL, depending on the person, there may be hardness up near the belly button, along with some pain/discomfort, bladder spasms, and leaking urine, especially during fundal checks. The only way to be certain how much urine is in the bladder though is to have a bladder scan done. An ultrasound bladder scanner is a portable device that uses ultrasonic reflections to assess urine retention postpartum.
Some specific reasons that postpartum urinary retention can occur are:
Pain, specifically in the perineum, can cause tension and the inability for the bladder to relax and release urine.
Fear, for example, if tearing or an episiotomy occurred near the urethra. Women who are afraid of the perinatal trauma and the pain that may occur with urination may consciously or subconsciously hold in their urine.
Swelling from a long second stage or baby’s head being in a funny position.
Prolonged second stage. According to the American College of Obstetricians and Gynecologists (ACOG), this is defined as the baby’s head being down and the mother’s cervix being dilated to 10cm for more than 3 hours in a first-time mom with an epidural, more than 2 hours in a first-time mom without an epidural, more than 2 hours in a repeat mother with an epidural, and more than 1 hour in a repeat mother without an epidural.
Loss of bladder sensation after childbirth.
Getting anesthesia, either general or regional, because of the location, also puts the bladder to sleep, while blocking labor/surgery pain. It can take a while for the bladder muscle to wake back up.
Loss of bladder tone and/or injury to the pelvic nerves aka “bladder nerves” during childbirth. Bladder nerve damage after childbirth can occur from stretching, straining, or tearing that happens during labor and delivery. When this happens, the signals that allow muscles to work properly are damaged or weakened, causing bladder problems after c section and epidurals.
Who may be most affected by Postpartum Urinary Retention?
To summarize who may be most affected by urine retention postpartum, here is a concise list of those shown to be more likely to experience urine retention after delivery.
Women delivering their first baby. The first time the pelvic floor muscles experience childbirth, they are being stretched and strained more than they ever have before. This can increase the likelihood of urine retention postpartum.
Women who have anesthesia when giving birth, either vaginally or via c-section.
Women who have forceps or vacuum extractions during vaginal deliveries.
Women who experience perineal trauma in the form of tearing or episiotomy.
Women who push for a long time.
How do you treat Postpartum Urinary Retention?
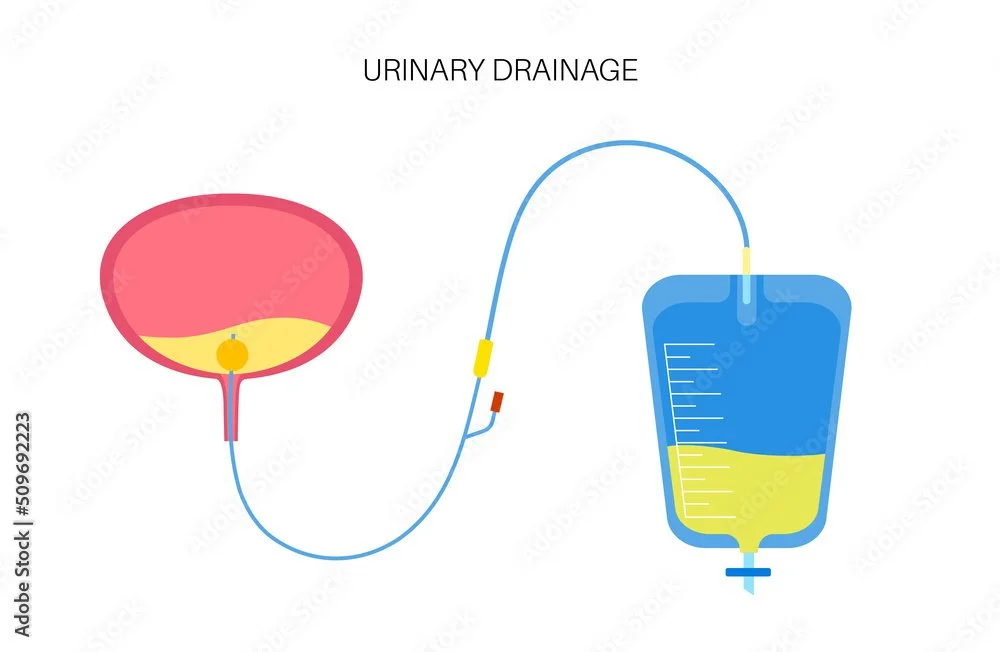
Since short-term postpartum urinary retention is fairly common, there are some tips you can try to help your body urinate naturally. However, the first line of treatment for postpartum urinary retention is usually a Foley catheter after birth is placed to give the bladder some rest and keep it empty. The care team will keep a close eye on how much urine drains into the drainage bag, and what color it is. Once the catheter is removed, you will be given a set amount of time to go on your own.
How long does Postpartum Urinary Retention last?
Most women are found to regain bladder function within the first 3 days postpartum, with most other cases resolving within 7 days postpartum. Persistent urinary retention beyond day 3 is rare. In the chance that the postpartum urinary retention persists, you may be given a clean intermittent catheterization (CIC) or intermittent self-catheterization (ISC) to perform yourself. In this case, your care team will show you how to properly use the device and will give you safety precautions.
Summary
Though peeing after birth can be difficult and uncomfortable, just remember to communicate with your care team every step of the way. Try utilizing my tips to help yourself, and ask lots of questions if interventions are needed. Knowledge is power, and you cannot be too informed when it comes to your body. You’ve got this momma!
Sources:
https://www.ncbi.nlm.nih.gov/books/NBK549844/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6022424/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4065200/
https://www.ncbi.nlm.nih.gov/books/NBK538497/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9206615/
https://www.ajog.org/article/S0002-9378(22)00631-7/fulltext
https://my.clevelandclinic.org/health/treatments/15434-clean-intermittent-catheterization